RTM CPT Codes 2026: Complete Guide for Physical Therapists to Maximize Reimbursement
Introduction
Remote Therapeutic Monitoring (RTM) is rapidly becoming an essential tool for physical therapists and other clinicians who want to extend care beyond the clinic. In 2026, Medicare expanded RTM CPT codes to enhance accessibility and reimbursement opportunities. Unlike Remote Patient Monitoring (RPM), RTM focuses specifically on therapy adherence, musculoskeletal status, and patient progress. These codes allow clinicians to bill for both device setup and ongoing treatment management, making remote care financially sustainable. The addition of new codes like 98985 and 98979 provides flexibility for shorter monitoring periods and brief patient interactions. Understanding these codes ensures accurate billing and compliance with Medicare guidelines. Physical therapists can now integrate digital monitoring seamlessly into treatment plans. Proper documentation and interactive communication with patients are crucial to optimize reimbursement. This guide will break down each RTM CPT code for 2026. By the end, clinicians will be equipped to apply these codes confidently in their practice.
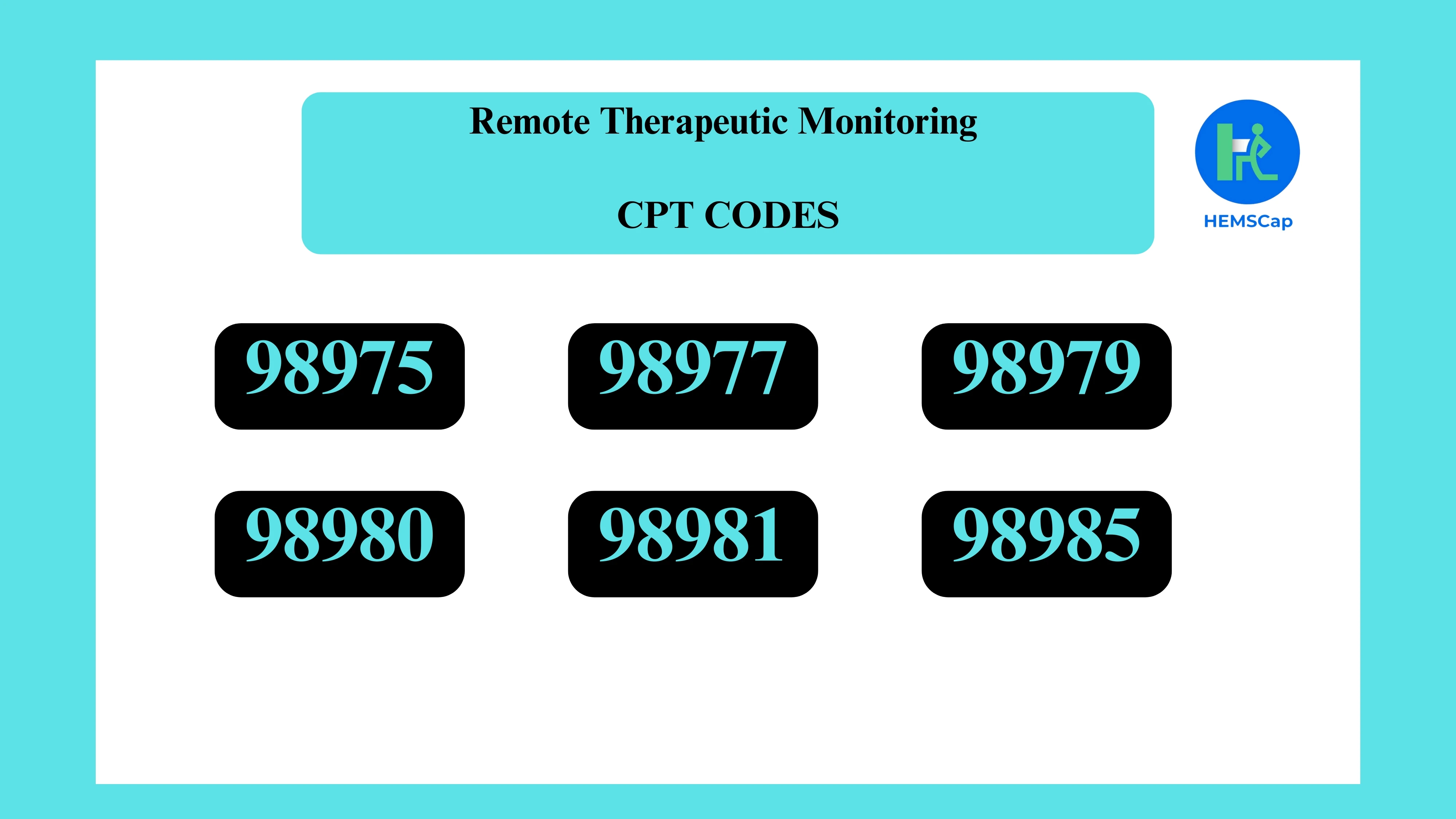
RTM CPT Codes and Descriptions (2026)
Remote Therapeutic Monitoring CPT codes define how clinicians are reimbursed for delivering and managing therapy outside of traditional in-clinic visits. In 2026, CMS expanded RTM billing options to better reflect real clinical workflows and patient engagement patterns. These codes separate device setup and data supply from ongoing treatment management, allowing more precise documentation and billing. Understanding when and how to apply each code is essential to avoid claim denials and ensure compliance. The table below summarizes the key RTM CPT codes for 2026, including their purpose, usage scenarios, and documentation requirements.
 What Each Code Means in Practice
What Each Code Means in Practice
CPT 98975 – Initial RTM Setup and Patient Education
This code reimburses clinicians for the time spent setting up RTM technology and teaching the patient how to use it effectively. Activities include:
- Configuring monitoring devices or software
- Educating patients on data capture and device usage
- Documenting patient understanding
CPT 98985 – RTM Supply (2–15 Days of Data)
Introduced in 2026, this code covers shorter monitoring periods of 2–15 days. Use it for patients requiring brief data collection, filling gaps left by longer-duration codes.
When to use:
- Short-term monitoring protocols
- Less intensive data collection scenarios
CPT 98977 – RTM Supply (16–30 Days of Data)
Reimburses for devices collecting musculoskeletal data over 16–30 days. Only one of 98985 or 98977 can be billed per 30-day period.
Requirement:
- ≥16 days of qualifying data transmitted
CPT 98979 – RTM Treatment Management (First 10 Minutes)
Covers the first 10 minutes of remote management, including at least one live interactive communication. Ideal for brief patient check-ins.
CPT 98980 – RTM Treatment Management (First 20 Minutes)
For the first 20 minutes of remote therapeutic management per month. Requires at least one interactive communication. Activities include reviewing RTM data and discussing treatment adjustments.
CPT 98981 – RTM Treatment Management (Additional 20 Minutes)
Used for additional 20-minute increments beyond 98980. Includes extended review of patient data and interactive communications.
RTM Code Categories (APTA)
The American Physical Therapy Association (APTA) groups RTM CPT codes into clear categories to help clinicians distinguish between device-related services and treatment management activities. This classification simplifies billing workflows and supports accurate documentation. By understanding these categories, physical therapists can better align clinical actions with appropriate codes. The table below outlines how RTM codes are organized according to APTA guidance.
 Clinical Documentation Best Practices
Clinical Documentation Best Practices
To ensure proper reimbursement, clinicians should document:
- Patient consent for remote monitoring
- Data transmission frequency and duration
- Interactive communications and clinical purpose
- Actions based on collected data
Adequate documentation supports compliance and reduces denied claims.
In addition to these core elements, documentation should clearly demonstrate clinical decision-making based on RTM data rather than passive data review. Notes should reflect how monitored information influenced treatment progression, patient education, or care plan adjustments. Clear time tracking for treatment management services is also critical, especially when billing time-based RTM codes. Consistent and detailed documentation not only supports reimbursement but also strengthens compliance during audits and payer reviews.
Integrating RTM into Clinical Workflows
Successfully implementing Remote Therapeutic Monitoring requires more than understanding CPT codes alone. Clinics must integrate RTM into existing workflows in a way that supports efficiency, clinical decision-making, and documentation accuracy. This includes selecting appropriate patients, defining monitoring duration, and assigning responsibility for data review and patient communication. When RTM is embedded into routine clinical processes, therapists can deliver consistent remote care while ensuring that billing and documentation requirements are met. Establishing clear internal protocols for RTM review helps prevent missed documentation and inconsistent billing. Training staff on time tracking and interactive communication requirements further reduces compliance risk. Over time, a standardized RTM workflow improves scalability and supports sustainable reimbursement.
Final Thoughts
Mastering RTM CPT codes for 2026 allows physical therapists to expand remote care efficiently and confidently. The new codes 98985 and 98979 provide flexibility for shorter monitoring and management sessions. Proper documentation, including live interactive communication, is critical to ensure Medicare compliance. Clinicians can now bill for setup, device supply, and treatment management accurately. Integrating RTM into clinical workflows helps track patient progress outside the clinic. These tools also improve patient engagement and adherence to therapy plans. PTs who adopt RTM benefit from better data-driven insights into treatment outcomes. Understanding both device and treatment management codes ensures complete reimbursement. Remote monitoring also reduces in-person visit dependency while maintaining care quality. Ultimately, RTM empowers therapists to deliver high-value, patient-centered care. Staying updated with code changes and best practices is essential for long-term success.
FAQ – Remote Therapeutic Monitoring CPT Codes
1. What is the difference between RTM and RPM codes?
RTM codes focus on therapy-related, non-physiologic data such as adherence, musculoskeletal status, and treatment response, while RPM tracks physiological data like heart rate or blood pressure.
2. Can physical therapists bill RTM codes under Medicare?
Yes, APTA confirms that PTs can bill Medicare for RTM codes when providing remote therapeutic monitoring services.
3. How do CPT 98985 and 98977 differ?
98985 is for 2–15 days of data collection, while 98977 is for 16–30 days. Only one code can be billed per 30-day period.
4. What qualifies as “interactive communication” for RTM billing?
Live communication with the patient or caregiver via phone, video, secure message, or in-person counts. It must be documented and clinically relevant.
5. Why is documentation important for RTM billing?
Accurate documentation ensures compliance, supports reimbursement, and provides a clear record of patient monitoring and treatment management activities.